更新说明
Artem Shmatko1,2,3,13, Alexander Wolfgang Jung2,4,5,6,13, Kumar Gaurav2,13, Søren Brunak4,7, Laust Hvas Mortensen5,7,8, Ewan Birney2 ✉, Tom Fitzgerald 2 ✉ & Moritz Gerstung1,2,9,10,11,12 ✉
Decision-making in healthcare relies on understanding patients’ past and current health states to predict and, ultimately, change their future course1–3. Artificial intelligence (AI) methods promise to aid this task by learning patterns of disease progression from large corpora of health records4,5. However, their potential has not been fully investigated at scale. Here we modify the GPT6 (generative pretrained transformer) architecture to model the progression and competing nature of human diseases. We train this model, Delphi-2M, on data from 0.4 million UK Biobank participants and validate it using external data from 1.9 million Danish individuals with no change in parameters. Delphi-2M predicts the rates of more than 1,000 diseases, conditional on each individual’s past disease history, with accuracy comparable to that of existing single-disease models. Delphi-2M’s generative nature also enables sampling of synthetic future health trajectories, providing meaningful estimates of potential disease burden for up to 20 years, and enabling the training of AI models that have never seen actual data. Explain able AI methods7 provide insights into Delphi-2M’s predictions, revealing clusters of co-morbid i ties within and across disease chapters and their time-dependent consequences on future health, but also highlight biases learnt from training data. In summary, transformer-based models appear to be well suited for predictive and generative health-related tasks, are applicable to population-scale datasets and provide insights into temporal dependencies between disease events, potentially improving the understanding of personalized health risks and informing precision medicine approaches.
医疗决策依赖于理解患者的过去和当前健康状况,以预测并最终改变其未来$病程^{1-3}$。人工智能 (AI) 方法有望通过从大量健康记录中学习疾病进展模式来辅助这一$任务^{4,5}$。然而,其潜力尚未得到大规模充分探索。本文我们修改 $GPT^6$ (生成式预训练 Transformer) 架构,以模拟人类疾病的进展和竞争性质。我们在来自 40 万英国生物银行参与者的数据上训练该模型 Delphi-2M,并使用来自 190 万丹麦个体的外部数据(参数未作任何更改)进行验证。Delphi-2M 在给定个体既往疾病史的条件下,预测超过 1,000 种疾病的发生率,其准确性与现有的单疾病模型相当。Delphi-2M 的生成特性还支持对合成未来健康轨迹进行采样,提供长达 20 年的潜在疾病负担的有意义估计,并使得训练从未见过真实数据的 AI 模型成为可能。可解释 AI 方法 7 提供了对 Delphi-2M 预测的洞察,揭示了疾病章节内部和跨章节的共病聚类及其对未来健康的时序依赖性后果,同时也凸显了从训练数据中学到的偏差。总之,基于 Transformer 的模型似乎非常适合预测性和生成性健康相关任务,可应用于人群规模的数据集,并提供对疾病事件间时间依赖关系的洞察,有可能改善对个性化健康风险的理解并为精准医疗方法提供信息。
The progression of human disease across age is characterized by periods of health, episodes of acute illness and also chronic debilitation, often manifesting as clusters of co-morbidity. Patterns of multimorbidity affect individuals unevenly and have been associated with lifestyle, heritable traits and socioeconomic status1–3. Understanding each individual’s multi-morbidity risks is important to tailor healthcare decisions, motivate lifestyle changes or direct entrance into screening programs, as is the case for cancer8,9. Critically, health cannot only be understood by the presentation of individual diagnoses but, rather, in the context of an individual’s co-morbid i ties and their evolution over time. While a wide range of prediction algorithms exist for specific diseases, from cardiovascular disease to cancer10–12, few algorithms are capable of predicting the full spectrum of human disease, which recognizes more than 1,000 diagnoses at the top level of the International Classification of Diseases, Tenth Revision (ICD-10) coding system.
人类疾病随年龄发展的特征表现为健康期、急性病发作期以及慢性衰弱期,通常以共病集群的形式呈现。多重病症模式对个体的影响存在差异,并与生活方式、遗传特征和社会经济地位$相关^{1-3}$。了解个体的多重病症风险对于定制医疗决策、推动生活方式改变或指导参与筛查项目至关重要,癌症筛查$案例^{8-9}$即是如此。关键的是,健康不能仅通过单一诊断表现来理解,而应结合个体的共病及其随时间演变的情境来考量。虽然现有针对特定疾病(从心血管疾病到$癌症^{10-12}$)的预测算法种类繁多,但能够预测人类全谱系疾病的算法寥寥无几——国际疾病分类第十版(ICD-10)编码系统顶层就包含逾千种诊断类别。
Learning and predicting patterns of disease progression is also important in populations that are ageing and that exhibit shifts in their underlying demographic’s morbid i ties. For example, it has been predicted that, globally, the number of cancer diagnoses will increase $77%$ by 2050 (ref. 13) or that, in the UK, the number of working-age individuals with major illnesses, including depression, asthma, diabetes, cardiovascular disease, cancer or dementia, will increase from 3 to 3.7 million by 2040 (ref. 14). Modelling the expected burden of disease is therefore critical for healthcare and economic planning and, moreover, the continual tracking of disease occurrence along with its likely future prevalence within population groups promotes a more informed healthcare system.
学习和预测疾病进展模式对于人口老龄化和基础人口发病率发生变化的人群也至关重要。例如,据预测,到2050年全球癌症诊断数量将增加77%(参考文献13);或在英国,患有重度疾病(包括抑郁症、哮喘、糖尿病、心血管疾病、癌症或痴呆症)的劳动年龄人口数量到2040年将从300万增至370万(参考文献14)。因此,模拟预期疾病负担对医疗保健和经济规划至关重要,此外,持续追踪疾病发生情况及其在人群中的未来可能患病率,有助于构建更知情的医疗保健系统。
Recent developments in AI may help to address some method o logical limitations of multi-morbidity modelling, which have so far proved difficult to overcome15. Aside from the great number of diagnoses, these include challenges in modelling temporal dependencies among previous events, the integration of potentially diverse prognostic ally relevant data and the statistical calibration of predictions. Large language models (LLMs)16–19—a subfield of AI that enables chatbots such as ChatGPT20,21—model language as a sequence of word fragments (tokens). Generated token by token, the new text is based on all preceding text
近期人工智能 (AI) 的发展可能有助于解决多病建模中一些难以克服的$方法学局限性^{15}$。除了诊断数量庞大之外,这些挑战还包括对既往事件间时间依赖性的建模、整合预后相关的多样化数据以及预测的统计校准。$大语言模型 (LLM)^{16–19}$——作为AI的一个分支领域,支撑了诸如$ChatGPT^{20,21}$等聊天机器人——将语言建模为词片段 (token) 的序列。新文本基于所有前文内容逐token生成。
and, with enough training, the statistical dependencies among these tokens prove sufficient to produce context-aware and even conversational text, which is often indistinguishable from that of a human counterpart.
并且,在足够的训练后,这些token之间的统计依赖性足以生成具有上下文感知能力甚至对话性的文本,其表现往往与人类生成的文本难以区分。
The analogy between LLMs and disease progression modelling, which also entails recognizing past events and exploiting their mutual dependencies to predict the future sequence of morbidity, has recently inspired a series of new AI models. For example, BERT-based models22–25 have been developed for specific prediction tasks. Transformer models trained on electronic health records have been used for predicting diagnoses such as pancreatic cancer26, self-harm25 and stroke24, as well as non-clinical parameters such as self-esteem27. However, despite promising proofs of concept4,28,29, the potential for comprehensive and generative multi-morbidity modelling has not yet been fully assessed.
大语言模型与疾病进展建模之间的类比,最近启发了一系列新的人工智能模型,这种类比也需要识别过去事件并利用它们的相互依赖关系来预测未来的发病序列。例如,基于$BERT的模型^{22–25}$已被开发用于特定的预测任务。在电子健康记录上训练的Transformer模型已被用于预测$胰腺癌^{26}$、$自残^{25}$和$中风^{24}$等诊断,以及$自尊心^{27}$等非临床参数。然而,尽管有前景的$概念验证^{4,28,29}$,全面和生成性多病建模的潜力尚未得到充分评估。
Here we demonstrate that attention-based transformer models, similar to LLMs, can be extended to learn lifetime health trajectories and accurately predict future disease rates for more than 1,000 diseases simultaneously on the basis of previous health diagnoses, lifestyle factors and further informative data. Our extended model, termed Delphi-2M, was trained on data from the UK Biobank, a population-scale research cohort, and validated on Danish population registries. The vocabulary of the model includes ICD-10 top-level diagnostic codes, as well as sex, body mass, smoking, alcohol consumption and death. Delphi provides individual-level predictions of multi-disease incidences and models future health trajectories at any point throughout an individual’s life course. Moreover, the internal model of Delphi offers insights into how past data influence the rates of subsequent diseases. We further assess biases and fairness across demographic subgroups and discuss Delphi’s potential as a framework for healthcare modelling.
在此我们证明,基于注意力的Transformer模型(类似于大语言模型)可扩展用于学习终身健康轨迹,并基于既往健康诊断、生活方式因素及其他信息数据,同时准确预测1000多种疾病的未来发病率。我们的扩展模型名为Delphi-2M,基于英国生物银行(一个大规模人群研究队列)的数据进行训练,并在丹麦人口登记库中完成验证。该模型的词汇表包含ICD-10顶级诊断代码,以及性别、体重、吸烟、饮酒和死亡信息。Delphi可提供个体层面的多疾病发病率预测,并对个体生命历程中任意时间点的未来健康轨迹进行建模。此外,Delphi的内部模型揭示了既往数据如何影响后续疾病发病率。我们进一步评估了人口统计学亚组间的偏差与公平性,并探讨了Delphi作为医疗建模框架的潜力。
A transformer model for health records
基于Transformer的健康记录模型
A person’s health trajectory can be represented by a sequence of diagnoses using top-level ICD-10 codes recorded at the age of first diagnosis as well as death. Furthermore, ‘no event’ padding tokens were randomly added at an average rate of 1 per 5 years to eliminate long intervals without other inputs, which are especially frequent for younger ages and during which the baseline disease risk can change substantially (Extended Data Fig. 1). Together, these data comprise 1,258 distinct states—tokens in LLM terminology. Additional information includes sex, body mass index (BMI) and indicators of smoking and alcohol consumption, which are used as input information but not predicted by the model (Fig. 1a).
个人的健康轨迹可以通过一系列诊断来表示,这些诊断使用首次诊断时记录的顶级ICD-10代码以及死亡信息。此外,平均每5年随机添加一个"无事件"填充标记 (padding token) ,以消除没有其他输入的长时间间隔,这种情况在年轻时尤其常见,且在此期间基线疾病风险可能发生显著变化 (扩展数据图 1) 。这些数据共同构成了1,258个不同的状态——即大语言模型 (LLM) 术语中的标记 (Token) 。附加信息包括性别、体重指数 (BMI) 以及吸烟和饮酒指标,这些信息用作模型的输入信息,但不由模型预测 (图 1a) 。
Training data comprised 402,799 $(80%)$ participants of the UK Biobank recorded before the 1 July 2020. Data for the remaining 100,639 $(20%)$ participants were used for validation and hyper parameter optimization, while all records for 471,057 $(94%)$ participants still alive on 1 July 2020 were used for longitudinal testing up until 1 July 2022 (Fig. 1b). Additional external testing was conducted on the Danish disease registry data, which covered 1.93 million Danish nationals and spanned the period from 1978 to 2018.
训练数据包含截至2020年7月1日前记录的402,799名$(80%$)英国生物银行参与者。其余100,639名$(20%$)参与者的数据用于验证和超参数优化,而截至2020年7月1日仍存活的471,057名$(94%$)参与者的所有记录被用于纵向测试至2022年7月1日 (图 1b) 。额外外部测试在丹麦疾病登记数据进行,该数据覆盖193万丹麦国民,时间跨度从1978年至2018年。
To model disease history data, which, in contrast to text, occurs on a continuous time axis, we extended the GPT-2 architecture 6 (Fig. 1c). Transformer models map their inputs into an embedding space, where information is successively aggregated to enable auto regressive predictions. The first change therefore replaces GPT’s positional encoding, a mapping that identifies each text token’s discrete position, with an encoding of continuous age using sine and cosine basis functions 16. Standard GPT models only predict the next token using a multi no mi al probability model. Thus, the second extension is the addition of another output head to also predict the time to the next token using an exponential waiting time model (Methods). Third, GPT’s causal attention masks, which ensure that the model accesses only information from past events, are amended to additionally mask tokens recorded at the same time. Padding, lifestyle and sex tokens use a similar encoding but do not enter the likelihoods, as the model is deliberately not trained to predict them.
为对疾病史数据进行建模(与文本不同,疾病史数据存在于连续时间轴上),我们扩展了GPT-2架构(图1c)。Transformer模型将其输入映射到嵌入空间,在该空间中信息被逐步聚合以实现自回归预测。因此,第一项改动是用基于正弦和余弦基函数的连续年龄编码,取代了GPT的位置编码(一种标识每个文本token离散位置的映射)。标准GPT模型仅使用多项概率模型预测下一个token。因此,第二项扩展是增加另一个输出头,使用指数等待时间模型也预测到下一个token的时间(方法部分)。第三,GPT的因果注意力掩码(确保模型仅访问过去事件的信息)被修改,以额外掩码在同一时间记录的token。填充token、生活方式token和性别token使用类似的编码,但不进入似然函数,因为模型被特意设计为不训练预测这些token。
We term this model Delphi (Delphi large predictive health inference). This architecture enables one to provide the model with a partial health trajectory (prompt in LLM terminology) to calculate the subsequent rate (per day) for each of the 1,256 disease tokens plus death. Furthermore, the next token and the time to this event can be sampled on the basis of these rates. Iterative ly, this procedure samples entire health trajectories (Fig. 1d).
我们将该模型称为Delphi (Delphi大型预测健康推理模型) 。该架构支持向模型输入部分健康轨迹 (即大语言模型术语中的提示) ,以计算1,256个疾病token及死亡事件的后续每日发生率。此外,基于这些发生率可采样下一个token及该事件的发生时间。通过迭代执行此过程,可采样完整的健康轨迹 (图1d) 。
A systematic screen of architecture hyper parameters (embedding dimensionality, number of layers, heads) confirms the reported empirical scaling laws30, which state that model performance increases with the number of datapoints and, up to a limit defined by the available data, as the number of parameters increases (Fig. 1e). The screen indicates that, for the UK Biobank dataset, optimal Delphi models have around 2 million parameters. One of the models within the optimal range has an internal embedding dimensionality of 120, 12 layers and 12 heads, amounting to a total of 2.2 million parameters. Results based on this model parameter iz ation are discussed throughout the rest of the paper. We note that qualitatively similar results are obtained from other parameter choices (Extended Data Fig. 2 and Supplementary Fig. 1).
对架构超参数 (嵌入维度、层数、头数) 的系统性筛选证实了已报道的经验缩放规律 [30] ,该规律指出模型性能随数据点数量提升,并在可用数据定义的限度内随参数数量增加而提升 (图 1e) 。筛选表明,对于 UK Biobank 数据集,最优的 Delphi 模型拥有约 200 万个参数。处于最优范围内的其中一个模型具有 120 的内部嵌入维度、12 层和 12 个头,总计 220 万个参数。本文其余部分将讨论基于此模型参数化的结果。我们注意到其他参数选择也可获得定性相似的结果 (扩展数据图 2 和补充图 1) 。
An ablation analysis shows how Delphi-2M architectural modifications contribute to a better age- and sex-stratified cross-entropy compared with a standard GPT model (Fig. 1f, Supplementary Table 1 and Supplementary Fig. 2). A good, albeit slightly inferior, classification performance at different ages may already be achieved by adding regular ‘no event’ padding tokens to the input data with GPT models alone. However, a key distinguishing feature of Delphi compared with basic GPT models is its ability to calculate the absolute rates of tokens, which provide consistent estimates of inter-event times (Fig. 1g). This property also implies that the rates may be interpreted as the incidences of tokens.
一项消融分析展示了Delphi-2M架构修改如何实现比标准GPT模型更优的年龄与性别分层交叉熵 (图 1f, 补充表 1 和 补充图 2)。仅通过向GPT模型的输入数据添加常规的"无事件"填充token,就可在不同年龄段实现良好(虽略逊一筹)的分类性能。然而,Delphi与基础GPT模型的关键区别在于其计算token绝对发生率的能力,这提供了事件间隔时间的一致性估计 (图 1g)。这一特性也意味着发生率可解释为token的发病密度。
Modelling multi-disease incidences
多疾病发病率建模
Delphi-2M’s accuracy in predicting diverse disease outcomes in the validation cohort is compared to the sex and age-stratified incidence as an epidemiological baseline. As can be seen in the ten examples shown in Fig. 2a, the incidence curves are very varied, with some diseases, such as chickenpox, peaking in infancy, while others, such as asthma or depression, are relatively flat and with most rising exponentially in old age. Moreover, there are noticeable differences between the sexes, which are obvious for breast cancer but also pronounced for diabetes, depression, acute myocardial infarction and death. Delphi-2M’s predictions are updated for each individual when new inputs are recorded. The predictions largely follow the sex- and age-stratified incidence curves but also indicate events or periods when the individual risk remains below or rises above the population average. For some diseases, such as asthma or arthrosis, the spread is narrow, indicating a limited ability to predict beyond the sex- and age-incidence trend. Yet for other diseases, including septic a emi a, and also death, the spread is wide, indicating predictable inter-individual differences in disease rates.
在验证队列中,将Delphi-2M预测多种疾病结局的准确性与按性别和年龄分层发病率作为流行病学基线进行比较。从图2a所示的十个示例可以看出,发病率曲线差异显著:有些疾病(如水痘)在婴儿期达到峰值,而其他疾病(如哮喘或抑郁症)的曲线相对平缓,且大多数疾病在老年期呈指数级上升。此外,性别间存在明显差异,这在乳腺癌中尤为突出,在糖尿病、抑郁症、急性心肌梗死和死亡中也很显著。当记录新的输入数据时,Delphi-2M会更新每个个体的预测结果。这些预测大体遵循性别和年龄分层的发病率曲线,同时能标示出个体风险低于或高于人群平均水平的特定事件或时期。对于某些疾病(如哮喘或关节病),预测分布范围较窄,表明超越性别和年龄发病率趋势的预测能力有限。然而对于其他疾病(包括败血症和死亡),预测分布范围较宽,表明疾病发生率存在可预测的个体间差异。
Delphi’s ability to predict the next diagnosis token across the spectrum of human disease is confirmed by the average age-stratified area under the receiver operating characteristic curve (AUC), which averages at values of approximately 0.76 in the internal validation data (Fig. 2b and Supplementary Table 2). For $97%$ of diagnoses, the AUC was greater than 0.5, indicating that the vast majority followed patterns with at least partial predictability. These patterns were found to be true across the different chapters of the ICD-10 spectrum, which define broad groups of disease for both sexes (Fig. 2c,d). Among the most confidently predicted next events is death, with an age-stratified AUC of 0.97 in both sexes. Importantly, calibration analyses in 5-year age brackets show that the predicted rates closely match the observed number of cases, showing that the models’ rates of the next tokens are consistently estimated (Extended Data Fig. 3).
Delphi 预测人类疾病谱系中下一个诊断 token 的能力通过平均年龄分层的受试者工作特征曲线下面积 (AUC) 得到证实,其在内部验证数据中的平均值约为 0.76 (图 2b 和补充表 2)。对于 $97%$ 的诊断,AUC 大于 0.5,表明绝大多数诊断遵循至少具有部分可预测性的模式。这些模式在 ICD-10 谱系的不同章节中均成立,这些章节定义了两性的广泛疾病组别 (图 2c,d)。在预测置信度最高的下一个事件中包括死亡,两性的年龄分层 AUC 均为 0.97。重要的是,5 岁年龄分组的校准分析表明,预测率与观察到的病例数高度匹配,显示模型对下一个 token 的比率估计是一致的 (扩展数据图 3)。
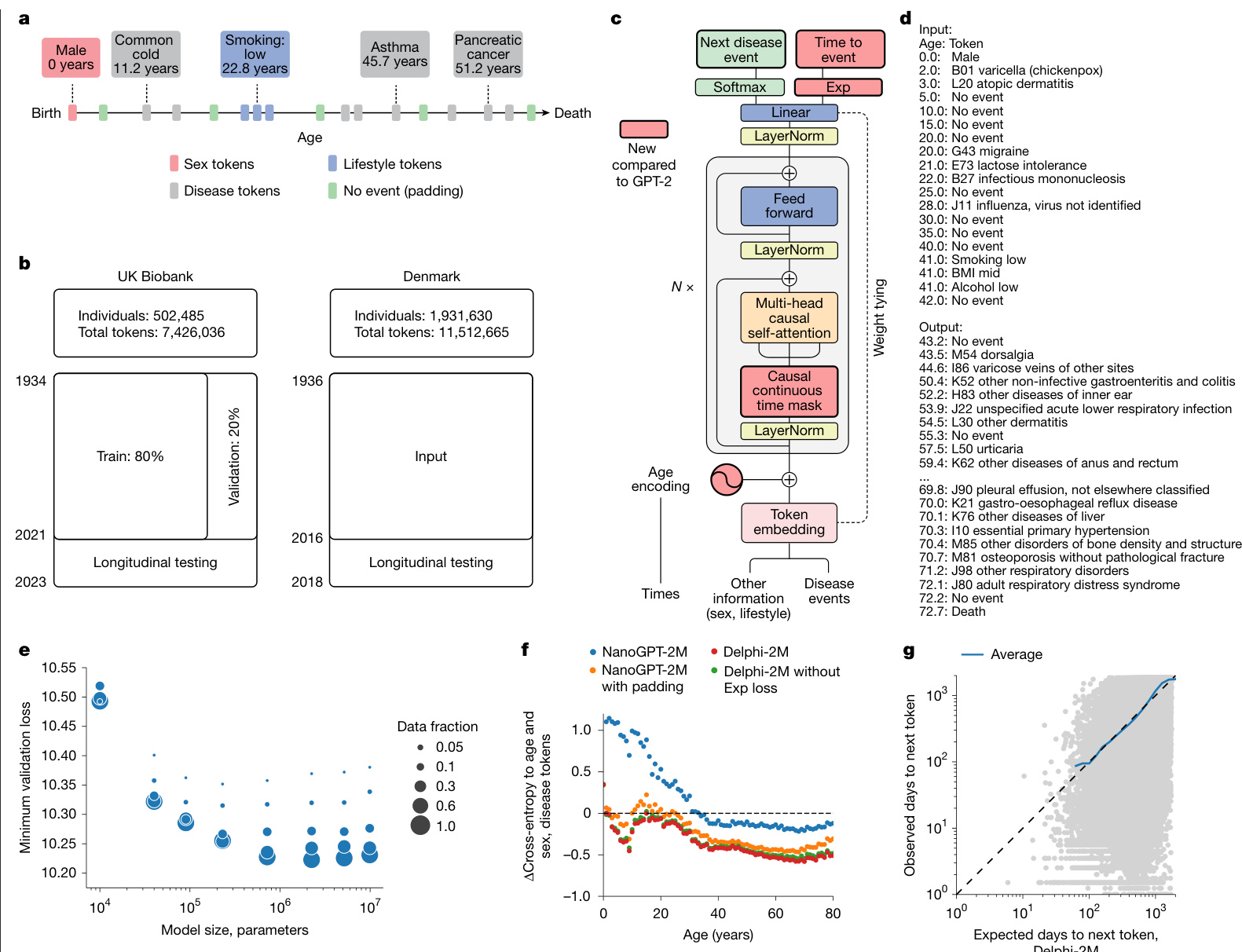
Fig. 1 | Delphi, a modified GPT architecture, models health trajectories. a, Schematic of health trajectories based on ICD-10 diagnoses, lifestyle and healthy padding tokens, each recorded at a distinct age. b, Training, validation and testing data derived from the UK Biobank (left) and Danish disease registries (right). c, The Delphi model architecture. The red elements indicate changes compared with the underlying GPT-2 model. $\mathbf{\nabla}^{\prime}N\times\mathbf{\nabla}^{\prime}$ denotes applying the transformer block sequentially N times. d, Example model input (prompt) and output (samples) comprising (age:token) pairs. e, Scaling laws of Delphi, showing the optimal validation loss as a function of model parameters for different training data sizes. f, Ablation results measured by the cross-entropy differences relative to an age- and sex-based baseline (y axis) for different ages (x axis). g, The accuracy of predicted time to event. The observed (y axis) and expected (x axis) time to events are shown for each next token prediction (grey dots). The blue line shows the average across consecutive bins of the x axis.
图 1 | Delphi,一种改进的 GPT 架构,用于建模健康轨迹。a,基于 ICD-10 诊断、生活方式和健康填充 Token 的健康轨迹示意图,每个记录对应不同年龄。b,来自英国生物银行(左)和丹麦疾病登记处(右)的训练、验证和测试数据。c,Delphi 模型架构。红色元素表示与底层 GPT-2 模型相比的更改。$\mathbf{\nabla}^{\prime}N\times\mathbf{\nabla}^{\prime}$ 表示顺序应用 Transformer 块 N 次。d,示例模型输入(提示)和输出(样本),包含(年龄:Token)对。e,Delphi 的缩放定律,显示了不同训练数据规模下,最佳验证损失随模型参数变化的函数关系。f,针对不同年龄(x 轴)的消融实验结果,以相对于基于年龄和性别的基线(y 轴)的交叉熵差异衡量。g,预测事件发生时间的准确性。对于每个下一个 Token 预测(灰点),显示了观察到的事件发生时间(y 轴)和预期的事件发生时间(x 轴)。蓝线显示了 x 轴连续分箱的平均值。
Next-event predictions are often the consequence of acute illness or diagnostic refinements that accrue over the course of a few weeks or months, which may be undesirable for prognostication. Delphi-2M’s average AUC values decrease from an average of 0.76 to 0.70 after 10 years, indicating that its predictions are also relevant for longterm prognostication (Fig. 2e and Supplementary Fig. 3). Similar results were observed in longitudinal test data, which also show no substantial shift in diagnostic patterns throughout the Biobank’s follow-up (Supplementary Fig. 4).
短期预后预测通常是急性疾病或在数周或数月内累积的诊断细化所导致的结果,这可能不利于预后评估。Delphi-2M 的平均 AUC 值在 10 年后从 0.76 降至 0.70,表明其预测同样适用于长期预后评估 (图 2e 和补充图 3) 。纵向测试数据中也观察到类似结果,这些数据同时显示生物样本库随访期间诊断模式未发生显著变化 (补充图 4) 。
The performance of Delphi was similar to routinely used clinical risk scores for cardiovascular disease and dementia, and better than those used for death. For diabetes, the performance of Delphi was worse compared with the use of a single marker, HbA1c, which is used clinically for risk prediction and diagnosis of diabetes (Fig. 2f, Supplementary Fig. 4c and Supplementary Table 3). This was the case for next-event predictions, as well as prediction horizons up to
Delphi的表现与心血管疾病和痴呆症的常规临床风险评分相当,且优于死亡风险评分。在糖尿病方面,Delphi的表现不如临床用于风险预测和糖尿病诊断的单一标志物HbA1c (图 2f、补充图 4c和补充表 3) 。这一结论适用于下次事件预测以及长达24个月的预测时间范围。
24 months. Delphi-2M’s AUC values were also generally higher than those of a recent machine learning algorithm that calculates the risks of a similarly broad spectrum of ICD-10 diagnoses using 67 different biomarkers available through the UK Biobank31, even though for many diagnoses, such as diabetes, biomarkers remain indispensable (Fig. 2e and Extended Data Fig. 4), marking potential for future modifications of Delphi that additionally use data beyond health records (Extended Data Fig. 5). For most cases, Delphi-2M’s multidisease predictions match or exceed current risk models for individual disease outcomes and offer the great advantage of enabling the simultaneous assessment of more than 1,000 diseases and their timing at any given time, while also surpassing multi-disease models in quality.
Delphi-2M的AUC值通常也高于最近的一种机器学习算法,该算法使用英国生物银行提供的67种不同生物标志物来计算类似广泛的ICD-10诊断风险31,尽管对于许多诊断(如糖尿病),生物标志物仍然不可或缺(图2e和扩展数据图4),这标志着Delphi未来修改的潜力,即额外使用健康记录之外的数据(扩展数据图5)。在大多数情况下,Delphi-2M的多疾病预测与当前针对单个疾病结局的风险模型相当或更优,并具有同时评估超过1,000种疾病及其在任何给定时间的时间点的巨大优势,同时在质量上也超过了多疾病模型。
Sampling future disease trajectories
采样未来疾病轨迹
One of the most promising features of generative models is the ability to sample disease trajectories, conditional on data recorded up to a certain point. This is a property that few conventional epi de mio logical models possess.
生成模型最有前景的特性之一是能够根据截至某个时间点所记录的数据,对疾病轨迹进行条件采样。这是传统流行病学模型很少具备的特性。
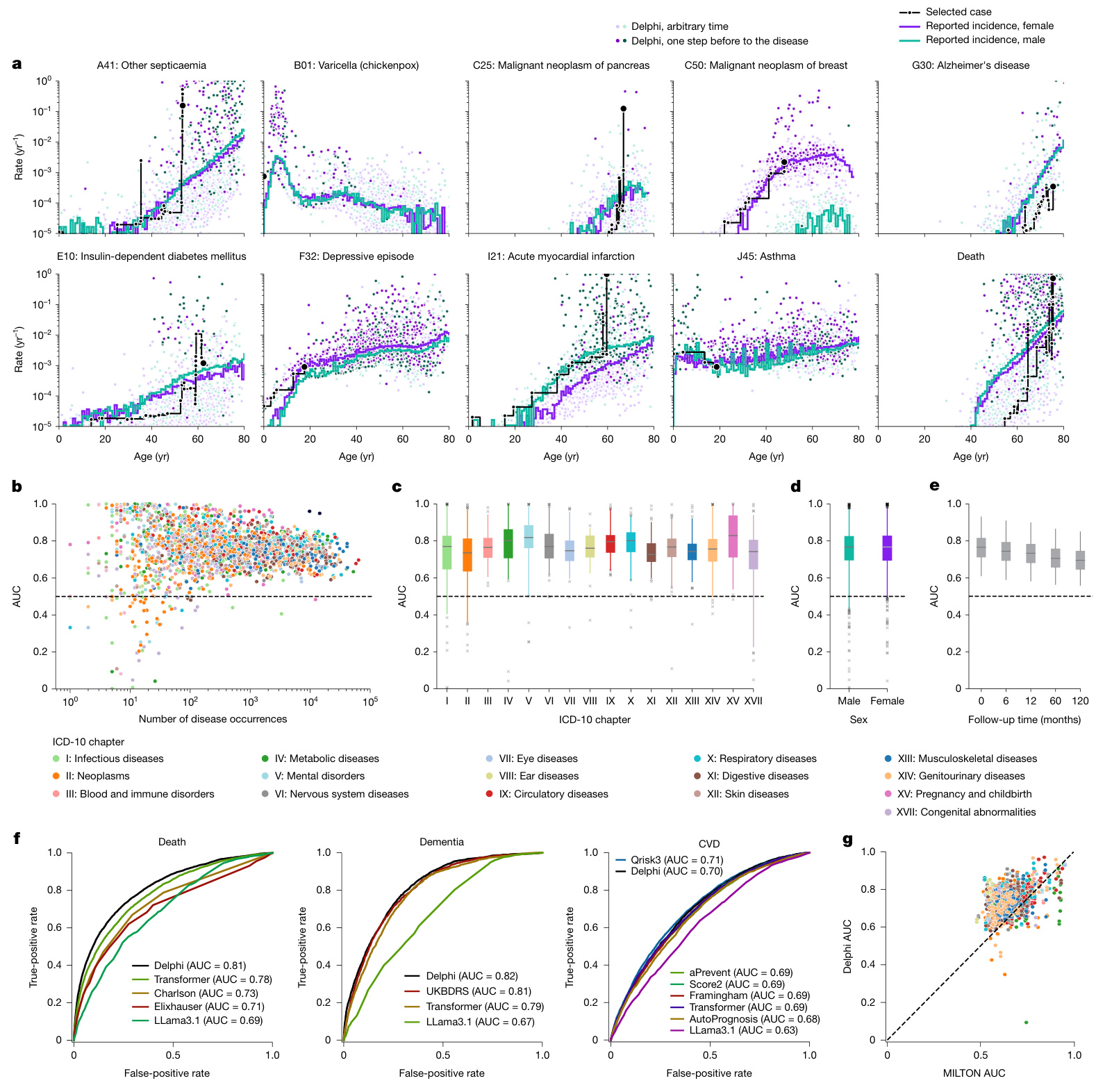
Fig. 2 | Delphi-2M accurately models the rates of a wide range of diseases. a, The predicted rates for nine exemplary diagnoses and death (y axis) as a function of age (x axis). The points show predictions at each recorded input token. Colours separate biological sex; the darker colours indicate predictions immediately before the diagnosis in question. The purple and turquoise lines are disease rates observed for each yearly age bin in the training data. The solid black line connects consecutive predictions for one randomly selected case throughout age. b, Average age–sex-stratified AUC values (y axis) as a function of training occurrences (x axis). Shown are data for $n=906$ diagnoses for male individuals and $n=957$ diagnoses for female individuals for which a sufficient number of events was recorded in the validation data to evaluate AUC values. c, The same as b, but aggregated by the ICD-10 chapter. d, The same as b, aggregated by sex. e, AUC values of all diagnoses in b for different time gaps between prediction and diagnoses (x axis). f, ROC curves for Delphi and other clinical or machine learning methods for three selected end points evaluated on the internal longitudinal testing set. g, AUC values of MILTON31, a biomarkerbased machine learning model (x axis), in prognostic mode, compared with Delphi-2M AUC values from the UK Biobank validation set (y axis) for $n=410$ diagnoses. The box plots in c–e show the median (centre line), the first to the third quartile (box limits) and the 0.025 and 0.975 quantiles (whiskers).
图 2 | Delphi-2M 精准模拟多种疾病的发生率。 a, 九项代表性诊断及死亡 (y轴) 的预测发生率随年龄 (x轴) 的变化关系。散点表示每个输入 token 对应的预测值。颜色区分生理性别;深色标示目标诊断发生前的预测值。紫色和青绿色线条为训练数据中各年龄分段的实际疾病发生率。黑色实线连接随机选取个案在整个年龄段的连续预测值。 b, 按年龄-性别分层的平均 AUC 值 (y轴) 随训练出现次数 (x轴) 的变化。数据显示男性 n=906 项诊断、女性 n=957 项诊断,这些诊断在验证数据中具有足够事件数用于评估 AUC 值。 c, 同 b, 但按 ICD-10 章节汇总。 d, 同 b, 按性别汇总。 e, b 中所有诊断在不同预测-诊断时间间隔 (x轴) 下的 AUC 值。 f, 在内部纵向测试集上评估三种重点结局时,Delphi 与其他临床或机器学习方法的 ROC 曲线。 g, 预后模式下基于生物标志物的机器学习模型 MILTON31 的 AUC 值 (x轴),与英国生物银行验证集中 Delphi-2M 对 n=410 项诊断的 AUC 值 (y轴) 对比。c-e 中的箱线图显示中位数 (中心线)、第一至第三四分位数 (箱体范围) 以及 0.025 和 0.975 分位数 (须线)。
To systematically assess the influence of medical histories on future health, we sampled health trajectories for each participant from the UK Biobank validation cohort on the basis of data available until the age of 60 years (Fig. 3a). This provides the opportunity to compare 63,662 sampled and observed trajectories. When evaluated at the population level, the disease incidences at ages 70–75 years are well recapitulated, showing that the overall distributions are well preserved by iterative sampling (Fig. 3b). This is further confirmed by the cross-entropy loss of sampled trajectories, which is, on average, indistinguishable from the observed data but drops when the preceding disease histories are shuffled between participants (Supplementary Fig. 5b).
为系统评估病史对未来健康的影响,我们根据截至60岁的可用数据,从英国生物银行验证队列中为每位参与者抽取了健康轨迹 (图 3a) 。这为比较63,662条抽样轨迹与观测轨迹提供了机会。在人群层面进行评估时,70-75岁的疾病发病率得到了良好再现,表明迭代抽样很好地保留了整体分布 (图 3b) 。抽样轨迹的交叉熵损失进一步证实了这一点,其平均值与观测数据无显著差异,但当参与者间的既往病史被打乱时该损失会下降 (补充图 5b) 。
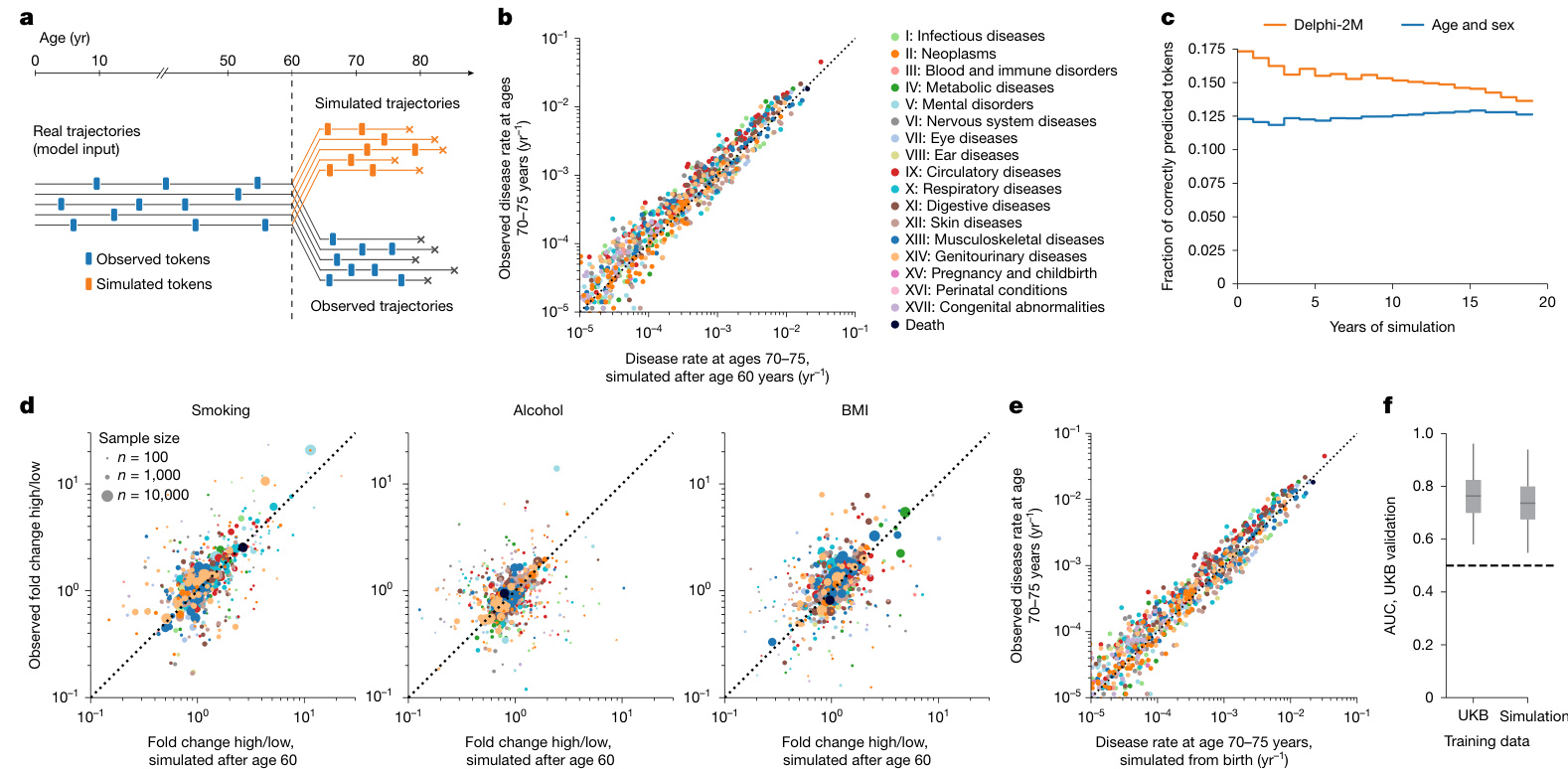
Fig. 3 | Generative modelling with Delphi-2M informs future outcomes. a, Schematic of the experiment design. Delphi-2M is used to simulate health trajectories using validation data $?n=63,622$ individuals with disease records both before and after 60 years of age) observed until the age of 60. A single trajectory is simulated per individual. Subsequently, simulated trajectories are compared to the observed outcomes for the same person. b, Delphi-2Mmodelled disease rates at ages 70–75 years (x axis) compared with observed rates at the same ages (y axis). c, The fraction of correctly predicted diagnoses (y axis) per 1-year age bin as a function of the years after simulation started at age 60 years (x axis). Delphi-2M, orange. The blue curve uses age and sex as a prediction baseline. d, Simulated (x axis) and observed (y axis) fold changes of disease rates for high versus low smoking, alcohol consumption and BMI groups. The evaluation period included ages 70–75 years and used simulations from the age of 60 years. e, The same as b, evaluated for simulations from birth. f, The AUC values of disease risk prediction $\scriptstyle(n=1,334$ disease–sex pairs) for Delphi when trained on UKB and Delphi-2M-sampled synthetic data (Methods). The box plots show the median (centre line), the first to the third quartile (box limits) and the 0.025 and 0.975 quantiles (whiskers).
图 3 | 使用 Delphi-2M 进行生成式建模预测未来健康结果。a, 实验设计示意图。Delphi-2M 被用于模拟健康轨迹,使用的验证数据为 $n=63,622$ 名在 60 岁前后均有疾病记录的个体,观测至 60 岁。为每个个体模拟一条轨迹。随后,将模拟轨迹与同一个体的实际观测结果进行比较。b, Delphi-2M 模拟的 70-75 岁疾病发生率 (x 轴) 与同年龄段实际观测发生率 (y 轴) 的对比。c, 在每个 1 岁年龄组中,正确预测的诊断比例 (y 轴) 随模拟从 60 岁开始后的年数 (x 轴) 的变化函数。Delphi-2M 为橙色曲线。蓝色曲线使用年龄和性别作为预测基线。d, 高吸烟量、高酒精摄入量和高 BMI 组与低水平组相比,疾病发生率的模拟倍数变化 (x 轴) 和观测倍数变化 (y 轴)。评估期为 70-75 岁,模拟从 60 岁开始。e, 与 b 相同,但评估的是从出生开始的模拟。f, 使用 UKB 数据和 Delphi-2M 生成的合成数据训练 Delphi 模型后,其疾病风险预测的 AUC 值 $\scriptstyle(n=1,334$ 个疾病-性别组合) (方法)。箱线图显示了中位数 (中心线)、第一至第三四分位数 (箱体界限) 以及 0.025 和 0.975 分位数 (须线)。
In the first year of sampling, there are on average $17%$ disease tokens that are correctly predicted, and this drops to less than $14%20$ years later. These figures compare to values of $12-13%$ of correctly predicted disease tokens using sex and age alone, confirming that the conditional generation helps to make more accurate predictions of future events (Fig. 3c and Supplementary Fig. 5c,d).
在采样第一年,平均有 $17%$ 的疾病标记被正确预测,20年后这一比例降至不足 $14%$。相比之下,仅使用性别和年龄的正确预测疾病标记比例为 $12-13%$,这证实了条件生成有助于更准确地预测未来事件 (图 3c 和补充图 5c,d)。
Delphi-2M’s ability to simulate differential health outcomes over a decade or more, on the basis of each individual’s health history, manifests in a multitude of ways. For example, the changes in disease burden in different population subsets defined by smoking, alcohol consumption or BMI are well predicted (Fig. 3d and Extended Data Fig. 6a). Similar findings are observed when the population is stratified by the presence of previous diseases or by estimated disease risks (Extended Data Fig. 6b,c). Together, these analyses show that Delphi-2M’s conditional samples provide meaningful extrapolations for future health courses, which reflect the influence of past health events.
Delphi-2M 基于个体健康史模拟十年或更长时间内差异化健康结果的能力体现在多个方面。例如,它能准确预测由吸烟、饮酒或体重指数 (BMI) 定义的不同人群亚组疾病负担的变化 (图 3d 和 扩展数据图 6a) 。当人群按既往疾病存在情况或估计疾病风险进行分层时,也观察到类似发现 (扩展数据图 6b,c) 。这些分析共同表明,Delphi-2M 的条件样本为未来健康轨迹提供了有意义的外推预测,这些预测反映了既往健康事件的影响。
The use of synthetic data has been proposed to help overcome issues with privacy in biomedical modelling if such datasets do not reveal characteristics specific to any one person. Fully synthetic data, which are sampled from birth with randomly assigned sex, reproduce the observed age and sex-specific incidence patterns throughout life (Fig. 3e). Further assessment shows that the generated trajectories do not exhibit any greater similarity to the training data than those from the validation cohort (Supplementary Fig. 6). While partially overlapping disease trajectories may be found in terms of absolute disease tokens, the extent of overlap appears as expected on the basis of the observed incidences and co-morbidity patterns.
使用合成数据已被提出,以帮助克服生物医学建模中的隐私问题,前提是这些数据集不泄露任何特定个体的特征。完全合成数据从出生时随机分配性别进行抽样,再现了整个生命周期中观察到的年龄和性别特异性发病模式 (图 3e) 。进一步评估表明,生成轨迹与训练数据的相似性并未超过验证队列中的轨迹 (补充图 6) 。虽然在绝对疾病 token 方面可能会发现部分重叠的疾病轨迹,但重叠程度与观察到的发病率和共病模式所预期的相符。
To illustrate the use of synthetic data, we trained a version of Delphi-2M exclusively on synthetic data. Notably, when evaluated on the observed validation data, the fully synthetically trained model achieves an age–sex-stratified average AUC of 0.74, which is only three percentage points lower than that of the original Delphi-2M model (Fig. 3f). This confirms that synthetic data preserve much of the information relevant to training Delphi models and may serve as a less privacy-sensitive alternative to personal data.
为了说明合成数据的用途,我们仅使用合成数据训练了一个Delphi-2M版本。值得注意的是,在观测验证数据上评估时,完全基于合成数据训练的模型实现了年龄-性别分层的平均AUC为0.74,仅比原始Delphi-2M模型低三个百分点 (图 3f) 。这证实了合成数据保留了训练Delphi模型所需的大部分相关信息,并可能作为个人数据的一种隐私敏感性较低的替代方案。
Explaining Delphi-2M predictions
Explaining Delphi-2M predictions
Insights into how Delphi-2M uses past information to predict future disease rates can be obtained by assessing the structure of the disease embeddings. GPT models linearly map inputs into a lower-dimensional embedding space, in which the temporal sequence of events is iteratively aggregated to produce a state from which predictions of each next token are derived (Fig. 1c). Delphi-2M’s specific implementation uses weight tying, which uses the same mapping to project the final embedding state to the token risks, guiding interpretation as the embedding matrix reflects the observed structure of co-morbidity risks.
深入了解Delphi-2M如何利用历史信息预测未来疾病率的关键在于评估疾病嵌入的结构。GPT模型将输入线性映射到低维嵌入空间,通过迭代聚合事件的时间序列生成状态,并基于该状态预测每个后续token(图1c)。Delphi-2M的具体实现采用权重绑定技术,使用相同映射将最终嵌入状态投射至token风险值。由于嵌入矩阵反映了观察到的共病风险结构,这一设计为模型解释提供了指导。
As shown by the uniform manifold approximation and projection (UMAP) representation of Delphi-2M’s embedding matrix in Fig. 4a, disease codes cluster closely by the underlying chapter, a property that the model has no direct knowledge of, and that purely reflects co-occurrence patterns in the data. Yet there are also noticeable exceptions, for example, cancers and precancers of the female reproductive tract. Another noteworthy cluster involves the two types of diabetes, retinal disorders and the n europ athies caused by them. Diseases with high acute mortality, such as myocardial infarction or septic a emi a, are clustering with death.
如图4a中Delphi-2M嵌入矩阵的均匀流形逼近与投影 (UMAP) 表示所示,疾病代码按底层章节紧密聚集,这一特性模型并未直接知晓,纯粹反映了数据中的共现模式。但也存在明显例外,例如女性生殖道癌症和癌前病变。另一个值得注意的簇涉及两种类型的糖尿病、视网膜病变及其引起的神经病变。急性死亡率高的疾病,如心肌梗死或败血症,与死亡聚集在一起。
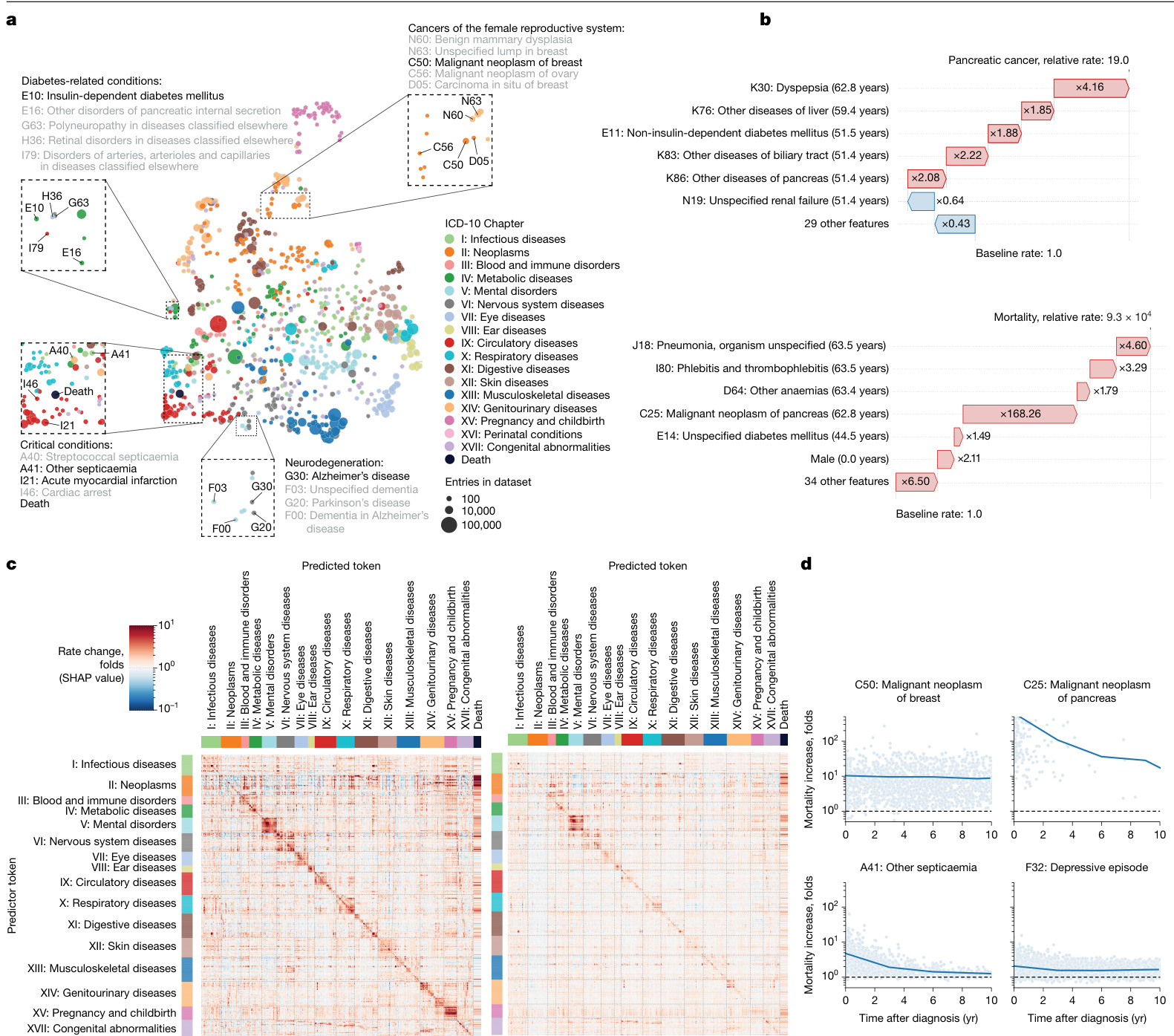
Fig. 4 | Explain able AI offers insights into disease progression. a, UMAP projection of token embeddings. Selected diseases are shown in the magnified areas. Colours define disease chapters. b, SHAP-explained token risk contributions for individual trajectories. Top, the risk of pancreatic cancer immediately before diagnosis at age 68.2 years, which was found to be $19\times$ increased. Bottom, the SHAP estimates of contributions to estimated mortality at age 63.5 years, which was greatly increased, in large part due to the preceding diagnosis of pancreatic cancer. c, The average SHAP effect of each of $n=778$ disease tokens with more than 5 occurrences and grouped by chapter (y axis) on the same set of tokens plus death (x axis). The red colours indicate a risk increase, whereas blue indicates a decrease. d, Rate change (SHAP value) of mortality (y axis) as a function of time after diagnosis (x axis) for selected diseases.
图 4 | 可解释人工智能为疾病进展提供洞察。a, Token嵌入的UMAP投影。放大区域显示了选定的疾病。颜色代表疾病章节。b, 针对个体轨迹的SHAP解释的Token风险贡献。上图显示在68.2岁诊断胰腺癌前的即时风险,发现增加了19倍。下图显示在63.5岁时对估计死亡率的SHAP贡献评估,该风险大幅增加,主要归因于先前诊断的胰腺癌。c, 按章节分组(y轴)的n=778个出现超过5次的疾病Token对同一组Token及死亡(x轴)的平均SHAP效应。红色表示风险增加,蓝色表示风险降低。d, 选定疾病的死亡率变化率(SHAP值)(y轴)随诊断后时间(x轴)的函数关系。
To gain further insights into how individual tokens influence future risks, shapley additive explanations (SHAP) values measure the influence of each token from the input trajectory on model predictions by a systematic assessment of subsampled data for individual prediction. As illustrated with the example of the proband’s partial trajectory shown in Fig. 4b, this analysis reveals that a series of disease diagnoses of the digestive tract (ICD-10 chapter XI) elevated their pancreatic cancer risk 19-fold. The subsequent pancreatic cancer diagnosis in turn increased the rate of mortality almost ten thousandfold.
为了进一步了解单个Token如何影响未来风险,沙普利加和解释 (SHAP) 值通过系统评估个体预测的子采样数据,来衡量输入轨迹中每个Token对模型预测的影响。如图 4b 所示的部分先证者轨迹示例,该分析显示一系列消化道疾病诊断 (ICD-10 第十一章) 将其胰腺癌风险提升了19倍。随后的胰腺癌诊断又将死亡率提高了近万倍。
SHAP analysis of data from 100,639 individuals of the validation cohort reveals the mutual dependencies by which each disease, sex and lifestyle token influences the rate of subsequent disease tokens, similar to hazard ratios in conventional statistical models (Fig. 4c (left)
对验证队列中 100,639 名个体数据的 SHAP 分析揭示了每种疾病、性别和生活方式标记影响后续疾病标记发生率的相互依赖关系,类似于传统统计模型中的风险比 (图 4c (左) )
and Extended Data Fig. 7). Effects mostly increase the rates of other diseases and are usually found among diseases of the same ICD-10 chapters, underscoring that the recorded patterns of co-morbid i ties often cluster within specific ICD-10 disease chapters. Particular clusters spanning entire disease chapters are visible for ICD-10 chapters V (mental disorders) and XV (pregnancy and childbirth). Notably, such patterns often appeared symmetrical, indicating similar predicted effect sizes of one disease token influencing another and vice versa (Supplementary Fig. 7). This behaviour can be attributed to the structure of the embedding space, which places temporarily co-occurring diagnoses in local proximity (Extended Data Fig. 8).
以及扩展数据图 7) 。影响主要表现为其他疾病发生率的提升,且通常集中在同一ICD-10章节的疾病范畴内,这说明记录到的共病模式往往聚集在特定的ICD-10疾病章节中。在ICD-10的第五章 V (精神障碍) 和第十五章 XV (妊娠和分娩) 中可见横跨整个疾病章节的特定聚集区。值得注意的是,这类模式常呈现对称性,表明某一疾病表征对另一疾病的影响预测规模具有双向相似性 (补充图 7) 。该现象可归因于嵌入空间的结构特性——该结构会将暂时性共现的诊断安置在相邻区域 (扩展数据图 8) 。
The patterns of modelled influences after 10 years are similar to short-term effects, even though the strength of associations is greatly a, Comparison between AUC values in the UKB longitudinal testing and the external testing using Danish data. b, Yearly mortality estimates by Delphi-2M (UK validation cohort), observed rates in the UK Biobank and Office for National Statistics national estimates across the entire British population. As only living individuals between 40 and 70 years of age (black line) were recruited to the UK Biobank, many deaths are missing compared with the Office for National Statistics population estimate (grey shaded area). c, UpSet plot of disease data availability in the UK Biobank validation cohort $(n=100,639)$ (top). Bottom, the data source distribution for records per disease token (token position sorted). d, Data source distribution for records per disease token (token position sorted). e, Hospital-record missing ness bias (relative rate after first hospital token; y axis) as a function of token exclusivity to hospital records (x axis) for each relevant diagnosis (points). Points are coloured by the ICD-10 chapter, the overall trend is shown in black using a non parametric (loess) curve with $95%$ confidence intervals shown in grey (UK validation cohort). f, Primary care missing ness bias (y axis) as a function of primary care token exclusivity, coloured by the ICD-10 chapter. The trend is shown in black using a non parametric (loess) curve with $95%$ confidence intervals shown in grey (UK validation cohort). g, SHAP value matrix, similar to Fig. 4c. The columns and rows correspond to different diseases and are sorted by the dominating source, then ICD-10 chapter. A dominating source is defined as the origin of more than $65%$ of records for a given disease; diseases without a dominating source are not shown. SHAP values indicate the greater influence of diseases on other diseases from the same group. SR, self-reported.
a, 英国生物银行纵向测试与使用丹麦数据的外部测试之间的AUC值比较。
b, Delphi-2M对英国验证队列的年度死亡率估计、英国生物银行观察到的死亡率以及英国国家统计局对全英人口的全国估计。由于英国生物银行仅招募了40至70岁的在世个体(黑线),与英国国家统计局的人口估计(灰色阴影区域)相比,许多死亡案例未被记录。
c, 英国生物银行验证队列 $(n=100,639)$ 中疾病数据可用性的UpSet图(顶部)。底部为每个疾病token(按token位置排序)的记录数据源分布。
d, 每个疾病token(按token位置排序)的记录数据源分布。
e, 医院记录缺失偏倚(首次医院token后的相对比率;y轴)与每个相关诊断(点)的医院记录token排他性(x轴)的函数关系。点按ICD-10章节着色,整体趋势通过非参数(loess)曲线以黑色显示,灰色区域表示 $95%$ 置信区间(英国验证队列)。
f, 初级护理缺失偏倚(y轴)与初级护理token排他性的函数关系,按ICD-10章节着色。趋势通过非参数(loess)曲线以黑色显示,灰色区域表示 $95%$ 置信区间(英国验证队列)。
g, 类似于图4c的SHAP值矩阵。列和行对应不同疾病,并按主导来源和ICD-10章节排序。主导来源定义为某疾病超过 $65%$ 记录的来源;未显示无主导来源的疾病。SHAP值表明同组疾病对其他疾病的影响更大。
SR表示自我报告。
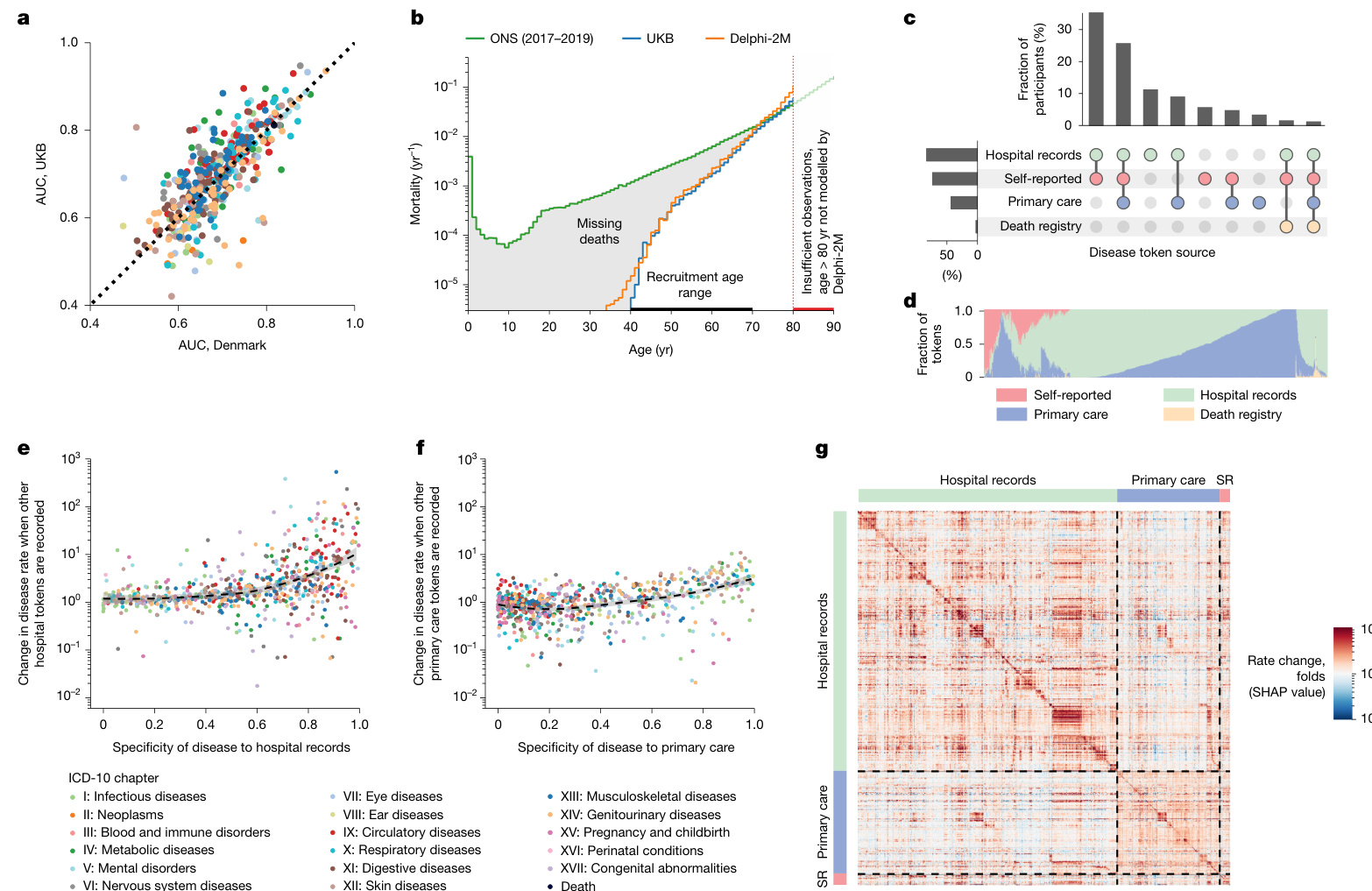
Fig. 5 | Epidemiological biases in UK Biobank data reflected by Delphi-2M.
图 5 | Delphi-2M 反映的英国生物样本库数据中的流行病学偏差。
attenuated (Fig. 4c (right)). The cluster relating to diseases of ICD-10 chapter XV (pregnancy and childbirth) within 5 years is entirely absent after 10 years, which is expected given that pregnancy-associated diseases occur within a finite period. However, dependencies among mental disorders remain apparent, similar to the effects of neoplasms on mortality. These observations are noteworthy as the quant if i cation of temporal dependencies on past events poses a particular challenge for conventional epidemiological models, whereas Delphi-2M’s GPT model uses attention-based weights, which are updated with every new input, including the ‘no event’ paddings.
在10年后完全消失(图4c(右))。与ICD-10第十五章(妊娠和分娩)相关的疾病簇在5年内出现,但在10年后完全消失,这是预期的,因为妊娠相关疾病发生在有限的时间内。然而,精神障碍之间的依赖性仍然明显,类似于肿瘤对死亡率的影响。这些观察值得注意,因为对过去事件的时间依赖性的量化对传统流行病学模型构成了特殊挑战,而Delphi-2M的GPT模型使用基于注意力机制的权重,这些权重会随着每个新输入(包括“无事件”填充)而更新。
To further illustrate Delphi-2M’s capabilities of modelling temporal dependencies, we note that, for some diseases, such as cancers, the influence on mortality decays with a half-life of several years, reflecting the sustained risks of recurrence or impacts of treatment (Fig. 4d). However, for septic a emi a, the influence on mortality is much more short-lived and drops sharply, effectively recovering to values close to the population average. This inference agrees with traditional Nelson–Aalen analyses of the hazard rates (Supplementary Fig. 8f). This behaviour is also reflected by Delphi-2M’s attention maps, which show that cancer tokens are attended to for long periods, while those of septic a emi a, myocardial infarction and many other diseases tend to be short lived (Supplementary Fig. 8).
为了进一步说明Delphi-2M建模时间依赖关系的能力,我们注意到对于某些疾病(如癌症),其对死亡率的影响会以数年半衰期逐渐衰减,这反映了疾病复发或治疗影响的持续风险(图 4d)。然而,对于败血症,其对死亡率的影响持续时间更短且急剧下降,能快速恢复至接近人群平均值的水平。这一推断与传统Nelson–Aalen风险率分析结果一致(附图 8f)。该行为也体现在Delphi-2M的注意力图谱中:癌症token会获得长期关注,而败血症、心肌梗死等疾病的注意力往往持续时间较短(附图 8)。
External validation and bias assessment
外部验证与偏差评估
To assess whether Delphi-2M’s inference generalizes to unseen cohorts, we performed external testing using Danish population registry data. For this purpose, we transferred Delphi-2M with the weights learned from the UK Biobank training and evaluated predictions on the Danish data; no retraining or adjustments have been made. The average AUC when Delphi-2M is applied to Danish data was 0.67 (s.d. 0.09), which is lower than for longitudinal testing on UKB data (0.69, s.d. 0.09). Predictions for different diseases were highly correlated across the datasets (Pearson correlation coefficient 0.76, $95%$ confidence interval (CI): 0.72–0.80) (Fig. 5a and Supplementary Fig. 9). The fact that Delphi-2M can be applied to Danish population data with slightly reduced accuracy indicates that many patterns learned by the model accurately reflect the true evolution of multi-morbidity,
为评估Delphi-2M的推理能力是否泛化至未见人群,我们使用丹麦人口登记数据进行了外部测试。为此,我们迁移了在UK Biobank训练中学习权重的Delphi-2M模型,并在丹麦数据上评估预测效果;未进行任何重新训练或调整。Delphi-2M应用于丹麦数据时的平均AUC为0.67(标准差0.09),低于UKB数据的纵向测试结果(0.69,标准差0.09)。不同疾病的预测结果在数据集间高度相关(皮尔逊相关系数0.76,95%置信区间(CI):0.72–0.80)(图5a和补充图9)。Delphi-2M能以略降低的准确率应用于丹麦人口数据的事实表明,模型学习到的许多模式准确反映了多病态演变的真实规律,
while also highlighting the existence of differences within each cohort.
同时强调每个群体内部存在差异。
A further question is to what extent a model trained on the UK Bio bank, which is an epidemiological cohort, generalizes to the general population. The UK Biobank comprises more white British citizens than the general population, and the participants tend to be on average more affluent and educated32. Lower rates of diseases are reported among participants of white ethnicity, and the rate of diagnoses increases with deprivation—trends that are reproduced by Delphi-2M (Extended Data Fig. 9). Further assessments of Delphi-2M’s performance in demographic subgroups are provided in the Supplementary Discussion, Supplementary Figs. 10 and 11 and Supplementary Table 4.
另一个问题是,基于英国生物银行 (UK Biobank) 这一流行病学队列训练的模型在多大程度上能推广到一般人群。英国生物银行中英国白人公民的比例高于普通人群,且参与者通常平均更富裕、受教育程度更高[32]。白人种族参与者的疾病报告率较低,而诊断率随贫困程度增加而上升——这些趋势均由Delphi-2M复现(扩展数据图9)。关于Delphi-2M在人口统计学亚组中表现的进一步评估见补充讨论、补充图10-11及补充表4。
In the UK Biobank, most individuals have been recruited between the ages of 40 and 70. This creates a selection bias, as no deaths are recorded before recruitment, which has direct implications for the estimated mortality (Fig. 5b). This immortality bias also indirectly affects the incidence of diseases associated with high mortality, such as cancers, as only survivors are included in the UK Biobank. For time-dependent analyses, the jump of mortality to non-zero values at recruitment can also lead to false attribution of the apparent increase to unrelated variables recorded at the time of recruitment. Furthermore, limited follow-up data are currently available for individuals 80 years of age and older. This period is therefore not reliably modelled by Delphi-2M.
在英国生物样本库中,大多数参与者的招募年龄在40至70岁之间。这造成了选择偏倚,因为在招募前没有死亡记录,这对估计死亡率有直接影响 (图 5b)。这种"永生偏倚"也间接影响高死亡率相关疾病(如癌症)的发病率,因为英国生物样本库仅包含幸存者。对于时间依赖性分析,死亡率在招募时跃升至非零值,也可能导致将明显增加错误归因于招募时记录的不相关变量。此外,目前对80岁及以上个体的随访数据有限。因此Delphi-2M无法可靠模拟这一时期。
UK Biobank’s disease data have been collated from self-reports, primary care, hospital admissions, cancer and death registries, each of which contributes characteristic disease tokens: self-reporting and GP records contain mostly common diseases, while data from hospital records include more-aggressive disease tokens, such as myocardial infarction or septic a emi a (Fig. 5d). However, the underlying sources were not always available for each participant and time period (Fig. 5c and Supplementary Fig. 12). Missing ness of a particular data source therefore causes the absence of multiple diagnoses. Such patterns, which reflect only the data-collection process, are also learned by Delphi-2M. The predicted rates of diseases exclusive to hospital records are, on average, ten times higher in individuals with a disease history that includes other hospital records (Fig. 5e,f). Septic a emi a, for example, is diagnosed in $93%$ of cases in a hospital setting and is predicted to occur at $8\times$ greater rates in individuals with any other hospital data. These source effects also explain some of the substructures visible in the UMAP representation of disease embeddings (Fig. 4a and Extended Data Fig. 10a–d) and also in the matrix of SHAP effects (Figs. 4c and 5g and Extended Data Fig. 10). While some of these associations may reflect true diagnostic pathways or disease clusters diagnosed in a distinct care setting, it nevertheless appears that some of these associations are artefacts stemming from the incomplete aggregated nature of the UK Biobank’s data.
UK Biobank的疾病数据来源于自我报告、初级保健、住院记录、癌症和死亡登记,每种数据源都贡献了特征性的疾病标记:自我报告和全科医生记录主要包含常见疾病,而住院记录数据则包含更具侵袭性的疾病标记,如心肌梗死或败血症 (图 5d)。然而,并非每位参与者和每个时间段都能获得基础数据源 (图 5c 和 补充图 12)。因此,特定数据源的缺失会导致多个诊断信息的缺失。Delphi-2M也学习了这种仅反映数据收集过程的模式。在包含其他住院记录病史的个体中,仅存在于住院记录中的疾病预测发生率平均高出十倍 (图 5e,f)。例如,败血症病例中有 $93%$ 在医院环境中诊断,并且预测在任何有其他住院数据的个体中发生率高出 $8\times$。这些数据源效应也解释了疾病嵌入的UMAP表示中可见的部分子结构 (图 4a 和 扩展数据图 10a–d) 以及SHAP效应矩阵中的部分结构 (图 4c、5g 和 扩展数据图 10)。虽然其中一些关联可能反映了真实的诊断路径或在特定护理环境中诊断的疾病集群,但似乎部分关联是由UK Biobank数据的不完整聚合性质所导致的人为现象。
Discussion
讨论
Here we present Delphi-2M—a GPT-based model of multi-disease progression. Delphi-2M extends the GPT large language model to account for the temporal nature of health trajectories. Analogous to LLMs, which learn the grammar and contextual logic of language from large bodies of text, Delphi-2M inferred the patterns of multi-disease progression when trained on data for more than 1,000 diseases and baseline health information recorded in 402,799 UK Biobank participants.
在此我们推出Delphi-2M——一个基于GPT的多疾病进展模型。Delphi-2M将GPT大语言模型 (Large Language Model) 扩展到健康轨迹的时间维度。类似于大语言模型从海量文本中学习语法和上下文逻辑,Delphi-2M在训练过程中通过402,799名英国生物银行参与者记录的1,000多种疾病及基线健康信息,推断出多疾病进展的模式。
A detailed assessment of Delphi-2M’s predictions showed that they consistently recapitulate the patterns of disease occurrence at the population scale as recorded in the UK Biobank. For the majority of diseases, Delphi-2M’s multi-disease, continuous-time model predicted future rates at comparable or better accuracy than established single-disease risk models, alternative machine learning frameworks and blood-biomarker-based models. Only a small performance drop was observed when applied to data from Danish disease registries, demonstrating that models are—even without additional finetuning— largely applicable across national healthcare systems.
对Delphi-2M预测能力的详细评估表明,其预测结果能持续复现英国生物银行(UK Biobank)记录的人群尺度疾病发生规律。对于大多数疾病,Delphi-2M的多疾病连续时间模型预测未来发病率的准确度达到或优于现有单疾病风险模型、其他机器学习框架及基于血液生物标志物的模型。在应用于丹麦疾病登记数据时仅观察到小幅性能下降,这表明该模型即使无需额外微调也基本适用于不同国家的医疗系统。
Delphi-2M is uniquely capable of sampling future disease trajectories, which enables the estimation of cumulative disease burdens over periods of up to 20 years, conditional on previous health information. Note that Delphi’s predictions are generally strongly influenced by statistical chance and compatible with a range of outcomes for a given individual. The ability to generate synthetic data may also help create datasets that preserve the statistical co-occurrence patterns without revealing any specific data, which could facilitate the development of further AI models with a decreased risk of revealing personal information.
Delphi-2M 具有独特的能力来模拟未来疾病轨迹,这使得它能够根据既往健康信息,估计最长20年内的累积疾病负担。需注意,Delphi的预测通常受统计概率的强烈影响,并且与特定个体可能出现的一系列结果相符。生成合成数据的能力还有助于创建保留统计共现模式而不泄露任何具体数据的数据集,这可以促进开发进一步的人工智能模型,同时降低泄露个人信息的风险。
Delphi-2M offers insights into the modes of disease progression. The ability to cluster disease risks may be useful for genomic association studies that focus on com or bidi ties or are stratified by the risks derived from health trajectories. Delphi-2M’s ability to quantify the temporal influence of previous health data revealed that cancers increase mortality in a sustained manner, while the effects of myocardial infarction or septic a emi a regress within 5 years. Similar analyses also revealed clusters of persisting com or bidi ties, such as mental health conditions. Although Delphi-2M appears to be capable of modelling temporally directed dependencies, we caution against interpreting these as causal relationships that could be exploited to modify future health courses.
Delphi-2M为疾病进展模式提供了新的见解。对疾病风险进行聚类的能力可能对关注共病或双向关联、或基于健康轨迹风险进行分层的基因组关联研究具有价值。Delphi-2M量化既往健康数据时间影响的能力显示,癌症会持续增加死亡率,而心肌梗死或败血症的影响在5年内消退。类似分析还揭示了持续性共病集群,例如心理健康状况。尽管Delphi-2M似乎能够建模时间导向的依赖关系,但我们提醒不要将其解释为可用来改变未来健康轨迹的因果关系。
There are also several limitations that need to be considered. A detailed analysis of UK Biobank’s first occurrence data revealed several biases, reflected by Delphi-2M. In addition to a healthy volunteer bias and participant selection bias before recruitment, the diverse nature of health data sources impacted Delphi’s prediction, as UK-Biobank-specific patterns of missing ness were exploited to infer disease rates. Furthermore, Delphi-2M predicts different disease rates in subgroups based on ancestry background and deprivation indices, but no observable trend between lifestyle measures and birth year. These findings underscore the need for caution when using AI models for inference and prediction in heterogeneous healthcare datasets, potentially marking them as useful additions to currently used diagnostic pipelines, rather than replacements.
还需考虑若干局限性。对英国生物银行首次发病数据的详细分析揭示了若干偏差,这些偏差在Delphi-2M中有所体现。除了招募前存在的健康志愿者偏差和参与者选择偏差外,健康数据来源的多样性也影响了Delphi的预测,因为模型利用了英国生物银行特有的缺失模式来推断疾病发生率。此外,Delphi-2M基于祖先背景和贫困指数预测了不同亚组的疾病发生率差异,但未发现生活方式指标与出生年份之间存在可观察的趋势。这些发现强调在异构医疗数据集中使用AI模型进行推断和预测时需要保持谨慎,或许应将其视为现有诊断流程的有益补充而非替代方案。
A promising feature of Delphi-2M’s implementation is the relative simplicity of incorporating additional data layers, rendered possible by the transformer-based architecture. Immediate refinements of Delphi-2M may incorporate additional lifestyle data, self-reported health status, prescription records and blood tests, all of which are usually available in a general healthcare setting. Further multimodal extensions could include genomic data, richer meta bol omi c information, diagnostic imaging data or data from wearables that can be added to Delphi-2M’s embedding layer, similar to how lifestyle tokens are currently incorporated (Extended Data Fig. 9). Furthermore, while ICD-10 provides a predefined token iz ation of diseases, LLMs have been shown to also conceptualize natural language, making it plausible to expect that future models may derive similar meaning directly from free text records, enabling the application of Delphi-like models to unstructured data. Lastly, Delphi-2M itself could serve as an extension to LLMs. Similarly to systems that provide LLMs with query-relevant web search results to reduce hallucinations 33, a future healthcare-oriented LLM could invoke a Delphi-based model to improve the numerical accuracy of the generated replies34.
Delphi-2M 实现的一个前景广阔的特性是,由于基于 Transformer 的架构,整合额外数据层相对简单。Delphi-2M 的即时改进可能纳入额外的生活方式数据、自我报告的健康状况、处方记录和血液检测结果,这些通常在常规医疗保健环境中可获得。进一步的多模态扩展可能包括基因组数据、更丰富的代谢组学信息、诊断影像数据或来自可穿戴设备的数据,这些都可以添加到 Delphi-2M 的嵌入层,类似于当前整合生活方式 Token 的方式(扩展数据图 9)。此外,虽然 ICD-10 提供了预定义的疾病标记化方法,但大语言模型已被证明也能概念化自然语言,因此可以合理预期未来的模型或许能直接从自由文本记录中推导出相似的含义,从而使得类似 Delphi 的模型能够应用于非结构化数据。最后,Delphi-2M 本身也可以作为大语言模型的扩展。类似于那些为大语言模型提供与查询相关的网络搜索结果以减少幻觉的系统 [33],未来面向医疗保健的大语言模型可以调用基于 Delphi 的模型,以提高生成回复的数值准确性 [34]。
An evident application of Delphi-type models is to support medical decision-making by rationally integrating information from various data modalities, which can be a challenge for healthcare professionals. Potential use cases could include identifying individuals who would benefit most from diagnostic tests or finding individuals with disease risk high enough to include them in screening programs, even if they have not yet met conventional age-based criteria. However, deploying clinical decision support systems requires a regulatory framework, which is still in its infancy for AI in healthcare.
Delphi型模型的一个明显应用是通过合理整合来自各种数据模态的信息来支持医疗决策,这对医疗专业人员来说可能是一个挑战。潜在的用例可能包括识别最能从诊断测试中受益的个体,或发现疾病风险足够高、可将其纳入筛查计划的个体,即使他们尚未达到传统的基于年龄的标准。然而,部署临床决策支持系统需要一个监管框架,而人工智能在医疗领域的监管框架仍处于起步阶段。
An alternative use of Delphi models would be to inform healthcare providers, insurers and policymakers. Such applications, which inform the provision of healthcare rather than treatment decisions, require less regulation. Delphi’s modelling has a resolution of an individual; when such predictions are aggregated, Delphi-type models may provide substantial system-wide modelling benefits, particularly in projecting the expected disease burden at local, regional and national levels, or for specific demographic groups of interest. This could reveal communities with unmet future healthcare needs over the next 1–2 decades and provide an opportunity to adjust the provision of healthcare. Such capabilities appear especially valuable in ageing populations in which healthcare needs are becoming increasingly complex and resource intensive.
Delphi模型的另一种用途是为医疗保健提供者、保险公司和决策者提供信息。这类应用于医疗保健服务而非治疗决策的场景,所需的监管较少。Delphi模型的分辨率可精确到个体;当此类预测被汇总时,Delphi类模型可带来显著的系统级建模优势,尤其在预测地方、区域和国家层面或特定关注人群的预期疾病负担方面。这能揭示未来10-20年医疗需求未得到满足的社区,并为调整医疗资源配置提供依据。这种能力在老龄化人口中显得尤为宝贵,因为其医疗需求正变得日益复杂且资源密集。
These considerations illustrate the wide range of applications of generative models for biomedical research and, ultimately, also for healthcare. With appropriate training and evaluation, future multimodal model extensions may be used for preventive medicine, clinical decision support and healthcare planning. Our model and analyses present a further step towards unlocking the considerable healthcare benefits of the era of AI.
这些考量展示了生成模型在生物医学研究乃至最终在医疗保健领域的广泛应用前景。通过适当的训练和评估,未来的多模态模型扩展可用于预防医学、临床决策支持和医疗保健规划。我们的模型和分析为推动实现人工智能时代巨大医疗效益迈出了新的一步。
Online content
在线内容
Any methods, additional references, Nature Portfolio reporting summaries, source data, extended data, supplementary information, acknowledgements, peer review information; details of author contributions and competing interests; and statements of data and code availability are available at https://doi.org/10.1038/s41586-025-09529-3.
任何方法、补充参考文献、Nature Portfolio报告摘要、源数据、扩展数据、补充信息、致谢、同行评审信息;作者贡献和竞争利益的详细信息;以及数据和代码可用性声明均可在 https://doi.org/10.1038/s41586-025-09529-3 获取。
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
出版方注:施普林格·自然对出版地图和机构附属关系中的管辖权主张保持中立。
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creative commons.org/licenses/by/4.0/.
开放获取 本文依据知识共享署名4.0国际许可协议授权 (http://creativecommons.org/licenses/by/4.0/) ,允许任何媒介或格式的使用、分享、改编、分发和复制,但须注明原作者及来源,提供知识共享许可协议链接并说明是否修改。文中图片或其他第三方内容均包含在知识共享许可协议中,除非素材署名中另有说明。若素材未包含在协议中且您的预期用途超出法定许可范围,请直接联系版权所有者获取授权。许可协议副本可访问 http://creativecommons.org/licenses/by/4.0/ 查看。
$\circledcirc$ The Author(s) 2025
$\circledcirc$ 作者 2025
Article Methods
文章方法
Data
数据
UK Biobank. Cohort. The UK Biobank is a cohort-based prospective study comprising approximately 500,000 individuals from various demographic backgrounds recruited across the UK between 2006 and 2010. At the time of recruitment, individuals were between 37 and 73 years of age35.
UK Biobank. 队列。UK Biobank是一项基于队列的前瞻性研究,包含2006年至2010年间在英国各地招募的约50万名来自不同人口背景的个体。在招募时,这些个体的年龄在37至73岁之间[35]。
Disease first occurrence data. The main data source for health-related outcomes is built on the first occurrence data assembled in category 1712 from the UK Biobank. These data include ICD-10 level 3 codes (for example, E11: type 2 diabetes mellitus) for diseases in chapters I–XVII, excluding chapter II (neoplasms), plus death. The data are pre-assembled by UK Biobank and include the first reported occurrence of a disease in the linked primary care data (cat. 3000), inpatient hospital admissions (cat. 2000), death registry (fields 40001 and 40002) or self-reported data through questionnaires (field 20002).
疾病首次发生数据。健康相关结局的主要数据源建立在英国生物样本库 (UK Biobank) 类别 1712 中汇总的首次发生数据基础上。这些数据包含 I–XVII 章节疾病(不包括第二章肿瘤)的 ICD-10 三级编码(例如 E11: 2型糖尿病)及死亡数据。数据由英国生物样本库预先汇总,包含关联初级诊疗数据(类别 3000)、住院数据(类别 2000)、死亡登记(字段 40001 和 40002)或通过问卷自我报告数据(字段 20002)中首次报告的疾病发生记录。
Information on neoplasms was not included in category 1712 by the UK Biobank, and we therefore included the data ourselves through the addition of the linked cancer registry data in fields 40005 and 40006 (subset to the first occurrence and mapped to ICD-10 level 3 codes), which, combined with first occurrence data, gives in total 1,256 distinct diagnoses. A list of all codes used is provided in Supplementary Table 5. Lifestyle and demographics. We extract information on the selfreported sex of participants as recorded in field 31 (indicators for female and male), a physical assessment of body mass index at recruitment from field 21001, which we split into three indicators encoding $\mathrm{BMI}<22\mathrm{kgm}^{-2}$ , $\mathrm{BMI}>28\mathrm{kgm}^{-2}$ and otherwise, as well as smoking behaviour from field 1239 with indicators for smoker (UKB coding: 1), occasionally smoking (2) and never smoker (0) and alcohol intake frequency from field 1558 with indicators for daily (1), moderately (2, 3) and limited (4, 5, 6). Furthermore, information that we extracted and used for stratification to assess model performance in subgroups but were not part of the data for model training include self-reported ethnic background (field 21000), with participants grouped into five level groups (white, mixed, Asian or Asian British, Black or Black British, and Chinese) and an index of multiple deprivation as available in field 26410. The index combines information across seven domains, including income, employment derivation, health and disability, education skills and training, barriers to housing and services, living environment and crime.
英国生物样本库的1712类别中未包含肿瘤相关信息,因此我们通过添加字段40005和40006中关联的癌症登记数据(限定为首次发生事件并映射至ICD-10三级编码)自行纳入数据,结合首次发生事件数据共获得1,256种独立诊断。所有使用编码列表见补充表5。生活方式与人口统计学特征。我们从字段31提取参与者自我报告的性别信息(女性和男性指标),从字段21001提取招募时体质指数的体格测量数据(将其划分为三个指标: $\mathrm{BMI}<22\mathrm{kgm}^{-2}$ 、 $\mathrm{BMI}>28\mathrm{kgm}^{-2}$ 及其他情况),从字段1239提取吸烟行为(吸烟者(UKB编码:1)、偶尔吸烟(2)和从不吸烟(0)的指标),从字段1558提取饮酒频率(每日饮酒(1)、适度饮酒(2、3)和有限饮酒(4、5、6)的指标)。此外,我们提取并用于分层评估模型在亚组中性能但未纳入模型训练数据的信息包括:自我报告的种族背景(字段21000,将参与者分为五类:白人、混血、亚洲或亚裔英国人、黑人或黑人英国人、华人)以及字段26410中的多重剥夺指数。该指数综合了收入、就业剥夺、健康与残疾、教育技能与培训、住房与服务障碍、居住环境与犯罪七个领域的信息。
Moreover, we extract information required for some of the algorithms we compare against. A list of the variables and their codes can be found in Supplementary Table 5.
此外,我们提取了部分对比算法所需的信息。相关变量及其代码列表可参见补充表 5。
Danish registries. Cohort. Exploring com or bidi ties and health-related factors is uniquely facilitated by Denmark’s comprehensive registries, which gather up to 40 years of interconnected data from across the entire population. All used registries are linkable through a unique personal identification number provided in the Central Person Registry along with information on sex and date of birth. Furthermore, we used the Danish National Patient Registry36 (LPR), a nationwide longitudinal register with data on hospital admissions across all of Denmark since 1977, along with the Danish Register of Causes of Death37 since 1970 to extract information on an individual’s acquired diagnoses throughout their lifetime. Our current data extract covers information up until around 2019 when reporting to the LPR was updated to LPR3. Furthermore, we restrict our cohort to individuals 50–80 years of age on 1 January 2016, to obtain a similar age range as in the UK Biobank. The 1 January 2016 was chosen as the cut-off point as it is the latest timepoint for which we can guarantee reliable coverage across the entire population over the entire prediction horizon.
丹麦登记系统。队列研究。丹麦的综合登记系统为探索合并症及健康相关因素提供了独特便利,该系统收集了全国人口长达40年的关联数据。所有使用的登记数据均可通过中央人口登记系统提供的唯一个人识别号进行关联,该识别号同时包含性别和出生日期信息。此外,我们使用了丹麦国家患者登记系统[36](LPR)——这是一个自1977年起覆盖丹麦全国医院住院数据的纵向登记系统,以及自1970年开始的丹麦死因登记系统[37],用以提取个体终生获得的诊断信息。当前数据提取涵盖至2019年左右的信息,当时LPR系统已更新至LPR3版本。我们将队列限制为2016年1月1日年龄在50-80岁之间的个体,以获得与英国生物银行相似的年龄范围。选择2016年1月1日作为截止点,是因为这是能保证在整个预测时间范围内获得全人群可靠数据的最新时间点。
Feature adjustments. To obtain a dataset that resembles the UK Biobank data, we retain only the first occurrence of an individual’s diagnosis and transform all codes to ICD-10 level 3 codes. Diagnoses before 1995 are reported in ICD-8 and have been converted to ICD-10 codes using published mappings38. Codes that may be present in the Danish register but were not in the UK Biobank are removed. Information on lifestyle is not available, and indicators for BMI, smoking and alcohol intake have therefore been treated as absent.
特征调整。为获得与英国生物银行数据相似的数据集,我们仅保留个体首次诊断记录,并将所有代码转换为ICD-10三级编码。1995年之前的诊断采用ICD-8编码,已通过公开映射表[38]转换为ICD-10代码。移除丹麦登记库中存在但英国生物银行未包含的代码。由于缺乏生活方式相关信息,BMI、吸烟和饮酒摄入指标均按缺失值处理。
Data splits. UK Biobank. The models were trained on UK Biobank data for 402,799 $(80%)$ individuals using data from birth until 30 June 2020. For validation, data contain the remaining 100,639 $(20%)$ individuals for the same period. Internal longitudinal testing was carried out using data for all individuals still alive by the cut-off date (471,057) and evaluated on incidence from 1 July 2021 to 1 July 2022, therefore enforcing a 1 year data gap between predictions and evaluation. Validation assesses how well the model generalized to different individuals from the same cohort. Longitudinal testing investigates whether the model’s performance changes over time and if it can be used for prognostic purposes. Denmark. External longitudinal testing was conducted on the Danish registries. All individuals residing in Denmark 50–80 years of age on the 1 January 2016 were included. Predictions are based on the available data up to this point and were subsequently evaluated on incidence from 1 January 2017 to 1 of January 2018, similar to the internal longitudinal testing. Data were collected for 1.93 million individuals ( $51%$ female and $49%$ male), with 11.51 million disease tokens recorded between 1978 and 2016. Predictions were evaluated on 0.96 million disease tokens across 796 ICD-10 codes (each with at least 25 cases).
数据划分。英国生物样本库。模型使用从出生至2020年6月30日的数据,对402,799名(80%)个体进行了训练。验证集包含同期剩余100,639名(20%)个体的数据。内部纵向测试采用截至截止日期仍存活的全部个体数据(471,057人),评估时段为2021年7月1日至2022年7月1日的发病率,确保预测与评估间存在1年数据间隔。验证旨在评估模型对同队列不同个体的泛化能力,纵向测试则探究模型性能随时间的变化及其预后适用性。丹麦数据集。外部纵向测试基于丹麦登记数据,纳入2016年1月1日年龄在50-80岁的全体丹麦居民。预测基于截至该时点的可用数据,评估时段为2017年1月1日至2018年1月1日的发病率,与内部纵向测试方案一致。共收集193万个体数据(女性51%,男性49),含1978至2016年间记录的1151万条疾病token。预测评估涵盖796个ICD-10编码(每个编码至少25例)下的96万条疾病token。
Model architecture
模型架构
GPT model. Delphi’s architecture is based on GPT-2 (ref. 6), as implemented in https://github.com/karpathy/nanoGPT. The basic GPT model uses standard transformer blocks with causal self-attention. A standard lookup table embedding layer with positional encoding was used to obtain the embeddings. The embedding and casual self-attention layers are followed by layer normalization and a fully connected feed forward network. Transformer layers, consisting of causal self-attention and feed forward blocks, are repeated multiple times before the final linear projection that yields the logits of the token predictions. The residual connections within a transformer layer are identical to those in the original GPT implementation. Here we also use weight tying of the token embeddings and final layer weights, which has the advantage of reducing the number of parameters and allowing input and output embeddings to be similarly interpreted.
GPT模型。Delphi的架构基于GPT-2(参考文献[6]),具体实现可参考https://github.com/karpathy/nanoGPT。基础GPT模型采用带因果自注意力机制的标准化Transformer模块。通过标准查找表嵌入层结合位置编码来获取嵌入向量。嵌入层和因果自注意力层后接层归一化及全连接前馈网络。由因果自注意力与前馈模块构成的Transformer层会重复多次,最终通过线性投影层输出Token预测的逻辑值。Transformer层内的残差连接与原始GPT实现保持一致。此处我们还采用了Token嵌入与最终层权重的绑定技术,其优势在于减少参数量,并使输入输出嵌入具有可类比性。
Data representation and padding tokens. Each datapoint consists of pairs (token, age) recording the token value and the proband’s age, measured in days from birth, at which the token was recorded. The token vocabulary consists of $n=1,257$ different ICD-10 level 3 disease tokens, plus $n=9$ tokens for alcohol, smoking and BMI, each represented by three different levels, as well as $n=2$ tokens for sex and $n=1$ no-event padding token as well as $n=1$ additional, non-informative padding token at the beginning or end of the input sequences.
数据表示与填充标记。每个数据点由 (标记, 年龄) 对组成,记录标记值以及标记被记录时参与者自出生起以天为单位的年龄。标记词汇表包含 $n=1,257$ 个不同的 ICD-10 3级疾病标记,加上 $n=9$ 个用于酒精、吸烟和 BMI 的标记(每个指标由三个不同等级表示),以及 $n=2$ 个性别标记、$n=1$ 个无事件填充标记,以及在输入序列开头或结尾添加的 $n=1$ 个无信息填充标记。
No-event padding tokens were added to the data with a constant rate of 1 per 5 years by uniformly sampling 20 tokens from the range of (0, 36525) and interleaving those with the data tokens after intersecting with the data range for each person. No-event tokens eliminate long time intervals without tokens, which are typical for younger ages, when people generally have fewer diseases and therefore less medical records. Transformers predict the text token probability distribution only at the time of currently observed tokens; thus, no-event tokens can also be inserted during inference to obtain the predicted disease risk at any given time of interest.
在数据中以每5年1个的恒定速率添加无事件填充token,具体方法是从 (0, 36525) 范围内均匀采样20个token,并与每个人的数据范围取交集后与数据token进行交错排列。无事件token消除了长时间间隔内没有token的情况(这在年轻年龄段尤为典型,因为人们通常患病较少且医疗记录较少)。Transformer 仅在当前观测到的token时间点预测文本token的概率分布;因此,在推理过程中也可插入无事件token,以获取任意指定时间点的预测疾病风险。
Sex tokens were presented at birth. Smoking, alcohol and lifestyle were recorded at the enrolment into the UK Biobank. As this specific time also coincided with the end of immortal time bias (probands had to be alive when they were recruited), smoking, alcohol and BMI tokens times were randomized by $^{-20}$ to $+40$ years from this point in time to break an otherwise confounding correlation leading to a sudden jump in mortality rates (and possibly other diseases with high mortality, such as cancers) associated with the recording of these tokens. This probably also diminishes the true effect of these tokens.
性别特征在出生时即已呈现。吸烟、饮酒及生活方式数据在参与者加入英国生物样本库时登记。由于该时间点也恰好对应永续时间偏倚的终止(研究对象入组时必须存活),我们将吸烟、饮酒和BMI特征的时间节点随机设定在此时间点的$^{-20}$年至$^{+40}$年范围内,以消除因记录这些特征导致的死亡率骤增(可能还包括癌症等高死亡率疾病)的混杂相关性。这种做法可能同时削弱了这些特征的真实效应。
Age encoding. Delphi replaces GPT’s positional encoding with an encoding based on the age values. Following the logic frequently used for positional encodings, age is represented by sine and cosine functions of different frequencies, where the lowest frequency is given by 1/365. These functions are subsequently linearly combined by a trainable linear transformation, which enables the model to share the same basis function across multiple encoding dimensions. Another advan tage of using age encoding is that Delphi can handle token inputs of arbitrary length, as no parameters are associated with token positions.
年龄编码。Delphi 将 GPT 的位置编码替换为基于年龄值的编码。遵循位置编码常用的逻辑,年龄通过不同频率的正弦和余弦函数表示,其中最低频率为 1/365。这些函数随后通过可训练的线性变换进行线性组合,使模型能够在多个编码维度共享相同的基函数。使用年龄编码的另一个优势是 Delphi 可以处理任意长度的 Token 输入,因为没有任何参数与 Token 位置相关联。
Causal self-attention. Standard causal self-attention enables the GPT model to attend to all preceding tokens. For sequential data, these are found to the left of the token sequence. Yet in the case of time-dependent data, tokens can be recorded at the same time with no specified order. Thus, attention masks were amended to mask positions that occurred at the same time as the predicted token. Non-informative padding tokens were masked for predictions of other tokens.
因果自注意力 (Causal self-attention) 。标准因果自注意力机制使 GPT 模型能够关注所有先前的 token。对于顺序数据,这些 token 位于 token 序列的左侧。然而在时间相关数据中,token 可能在同一时间被记录且没有特定顺序。因此,我们修改了注意力掩码,以屏蔽与预测 token 同时发生的位置。对于其他 token 的预测,非信息性的填充 token 会被屏蔽。
Exponential waiting time model. The input data to Delphi are bivariate pairs $(j,t)$ of the next token class and the time to the next token. Delphi is motivated by the theory of competing exponentials. Let $T_{i}$ be the waiting times from the current event to one of $i=1,$ , …, n competing events, where $n$ is the number of predictable tokens. Assuming the $T_{i}$ are each exponentially distributed waiting times with rates $\lambda_{i}=\exp(\log\mathrm{its}_{i})$ , the next event being j is equivalent to $T_{j}$ being the first of the competing waiting times, that is, $T_{j}=\operatorname*{min}T_{i},$ or equivalently j $=$ argmin $T_{i}.$ . It can be shown that the corresponding probability is $P(j=$ argmin $T_{i})=\lambda_{j}/\Sigma_{i}\lambda_{i},$ which is the softmax function over the vector of logits. Conveniently, this definition corresponds to the classical cross-entropy model for classification with $\lambda=$ exp(logits). Thus, Delphi uses a conventional loss term for token classification:
指数等待时间模型。Delphi的输入数据是下一个token类别与下一个token到达时间的二元组 $(j,t)$ 。Delphi的理论基础是竞争指数分布理论。设 $T_{i}$ 表示从当前事件到 $i=1,$ ..., $n$ 个竞争事件之一的等待时间,其中 $n$ 是可预测token的数量。假设每个 $T_{i}$ 都是指数分布的等待时间,其速率 $\lambda_{i}=\exp(\log\mathrm{its}_{i})$ ,则下一个事件为j等价于 $T_{j}$ 是竞争等待时间中的最小值,即 $T_{j}=\operatorname*{min}T_{i},$ 或等价于 j $=$ argmin $T_{i}.$ 。可以证明相应的概率为 $P(j=$ argmin $T_{i})=\lambda_{j}/\Sigma_{i}\lambda_{i},$ 这正是logits向量上的softmax函数。便利的是,该定义对应于经典的交叉熵分类模型,其中 $\lambda=$ exp(logits)。因此,Delphi采用常规的token分类损失项:
$$
\mathsf{l o s s}_{j}=-\mathsf{l o g}P(j)=-\mathsf{c r o s s_e n t r o p y}(\mathsf{l o g i t s},\mathsf{t o k e n s})
$$
$$
\mathsf{l o s s}_{j}=-\mathsf{l o g}P(j)=-\mathsf{c r o s s_e n t r o p y}(\mathsf{l o g i t s},\mathsf{t o k e n s})
$$
Furthermore, in the competing exponential model the time to the next event $T^{*}{=}\operatorname*{min}T_{j}$ is also exponentially distributed with rate $\lambda^{*}=$ $\varSigma_{i}\lambda_{i}=\varSigma_{i}\mathrm{exp}(\mathrm{logits}_{i})$ . The loss function of exponential waiting times $T$ between tokens is simply a log-likelihood of the exponential distribution for $T^{*}$ :
此外,在竞争指数模型中,下一事件的发生时间 $T^{*}{=}\operatorname*{min}T_{j}$ 也服从速率为 $\lambda^{*}=$ $\varSigma_{i}\lambda_{i}=\varSigma_{i}\mathrm{exp}(\mathrm{logits}_{i})$ 的指数分布。Token 间指数等待时间 $T$ 的损失函数即是指数分布对 $T^{*}$ 的对数似然:
$$
\mathrm{loss}_{T}=-\mathrm{log}p(T^{*})=-(\mathrm{logsumexp}(\mathrm{logits})-\mathrm{sum}(\mathrm{exp}(\mathrm{logits}))\times T^{*}).
$$
$$
\mathrm{loss}_{T}=-\mathrm{log}p(T^{*})=-(\mathrm{logsumexp}(\mathrm{logits})-\mathrm{sum}(\mathrm{exp}(\mathrm{logits}))\times T^{*}).
$$
These approximations hold as long as the rates $\lambda_{i}$ are constant in time, which is a reasonable assumption over short periods. For this reason, padding tokens were introduced to ensure that waiting times are modelled over a relatively short period, which does not exceed 5 years in expectation. In line with the tie-braking logic used for causal self-attention, co-occurring events were predicted from the last non-co-occurring token each.
只要速率 $\lambda_{i}$ 在时间上保持恒定(在短期内这是一个合理的假设),这些近似就成立。因此,引入了填充token来确保等待时间在相对较短的周期内建模,该周期预期不超过5年。与用于因果自注意力的平局决胜逻辑一致,共现事件各自从最后一个非共现token进行预测。
Loss function. The total loss of the model is then given by:
损失函数。模型的总损失由以下公式给出:
$$loss=loss_{j}+loss_{T}
$$
$$
$loss=loss_{j}+loss_{T}
$$
Non-informative padding, as well as sex, alcohol, smoking and BMI, were considered mere input tokens and therefore removed from the loss terms above. This was achieved by setting their logits to -Inf and by evaluating the loss terms only on disease and ‘no event’ padding tokens.
非信息性填充,以及性别、酒精、吸烟和BMI,仅被视为输入token,因此从上
